Diabetes Mellitus
Diabetes is a common condition in today’s world and is far too complex in what it is, how it impacts individuals and how it affects different organs and parts of your body to simply put into this blog. I will be briefly touching on what it is, the global burden of diabetes, how a podiatrist can help, symptoms you can experience, how it concerns the lower limb, and how you can prevent complications within the foot.
What is diabetes?
Diabetes is bracketed together with other metabolic diseases which is typified by hyperglycaemia (high blood sugars) developing from insulin deficiencies.
Prolonged hyperglycaemia and erratic blood sugar levels of
diabetes is linked with significant periods of damage, dysfunction, and numerous organ failure, in particular, eyes, kidneys, nerves, heart, and blood vessels.
Global burden of diabetes
Globally, diabetes has major implications on countries health systems. The International Diabetes Federation approximates back in 2015 that individuals aged between 20-79 years old, that is 1 in 11 adults has diabetes. This is forecasted further to rise in 2040 to 642
million in a recent article.
How can a podiatrist help
A podiatrist is the foot health expert, and is one of many health care professionals that can help after diagnoses is made through your GP. At the initial consult the podiatrist will take a thorough medical history and a series of tests and visual assessment to assess parameters and risks in relation to diabetic foot complications.
This will include assessing neurological, vascular status of the foot, lower limb foot deformities, skin texture/colour/temperature/integrity, and nail integrity. They will then devise an appropriate management plan according to your overall lower limb health to prevent diabetic complications and encourage foot health .
Symptoms a diabetic can experience
Peripheral neuropathy is where the nerves are damaged and you may develop paraesthesia (pins and needles), burning, sharp shooting or numbness sensations.
Typically these symptoms start in the toes and work upwards and once entrenched in the lower limb moves to the upper limbs and follows a glove and stocking pattern (starts off in the toes and moves up the foot/ankle and leg region and is equal on
both sides).
Motor neuropathy
Motor neuropathy is generally not present in the early phases of peripheral
neuropathy. Symptoms such as small muscle wasting, muscle atrophy and muscle weakness result in malformation of the foot which can increase the pressure areas under the foot often leading to callous or pressure ulcers . These tend to happen later in the disease process.
Autonomic neuropathy
Diabetic autonomic neuropathy (DAN) is among the least recognised and understood complications of diabetes despite its significant negative impact on survival and quality of life in people with diabetes.
There are a number of ways in which impairment of the autonomic supply to the foot could contribute to the formation of an ulcer. Impairment of autonomic function is responsible for the typical dry foot of a patient with neuropathy, and this may form a callus which presents in the area of high mechanical stress.
Peripheral arterial disease (PAD)
Intermittent claudication
Intermittent claudication, is where the calf muscle doesn’t enough oxygen needed to pump the muscle and elicited by mild ambulation, is one of the most debilitating clinical symptoms of peripheral vascular disease (PVD). The pain usually concentrates in the calves, precludes further walking, and only improves with rest.
Rest pain
Continuous burning sensation in the lower leg, which is relieved by sitting and aggravated by reclining/elevating the leg.
Critical limb ischemia
Critical limb ischaemia (CLI) means there is limb pain that happens at rest, or impending limb loss that is caused by severely weakened blood flow to the affected limb. PAD is a problem of supply vs demand, that means, insufficient blood flow to make available important oxygen demands from the limb. CLI occurs due to chronic lack of blood supply, which sets off a waterfall of disorganised physiological episodes that develop into rest pain or wounds in the legs, or both.
Acute limb-threatening ischaemia
Acute limb ischaemia is defined as a unexpected loss of limb, leading to ishaemic tissue injury and the resulting risk of limb loss. This is a medical emergency and requiring an immediate referral to Hospital.
Although rare, it is crucially important not to miss. It typically presents as sudden onset, indicated by the 6 Ps’:
Pain at rest
Pallor (flushed white colour skin)
Pulseless
Paraesthesia (pins and needles)
Paralysis (suddenly cannot walk)
Perishingly cold
*Only need to see a couple of these signs
Gait dysfunction
Studies have shown diabetic patients take shorter steps with a wider base of support, walk slower and have extended times of double support phase, limited ankle and knee mobility, lower plantar flexion moment and power than non-diabetic population. It can be said that some individuals with diabetes and peripheral neuropathy have a gait instability. This unsteady walking pattern can suggest lack of proprioception affecting the gait.
Complications associated to diabetes
Why do diabetic wounds occur?
Diabetic foot lesions happen due to a combination peripheral neuropathies, trauma and PAD. Neuropathy leads to insensate foot, sometimes deformed foot and can be accompanied with an abnormal gait pattern. In individuals with neuropathy, minor trauma (caused potentially by ill-fitting footwear, walking barefoot or an acute injury) can form a chronic ulcer. Loss of feeling, foot malformations and reduced joint mobility can cause irregular biomechanics loading of the foot. Thick skin (callus) forms as a result and this perpetuates the abnormal foot loading,
subcutaneous haemorrhage, skin breakdown and ulcer formation.
Neuropathic wounds
Presentation
Typically a punched out appearance which has surrounding callous around the wound. Generally seen on pressure areas of the foot which explains the callous surrounding the wound which is the bodies natural protective mechanism. If unnoticed, due to the loss of protective sensation and repetitive trauma the wound will progress quickly.

Features
Diminished or absent sensation to touch, pain, pressure or vibration. Patient has warm feet as the blood supply is not compromised. Prevalence around 35%.
Main issue
The lack of protective sensation due to pheripheral neuropathy over these pressure points will in turn lead to micro trauma which will break down the overlying tissue and subsequent wound.
Ischaemic wounds
Presentation
Presents as a punched out, with well defined round and even wound margins. Seen on bony prominences/high pressure areas/lateral gaiter region .

Features
Claudication, cold too touch, little to no pulse present, nil hair growth to the
affected limb, limb may turn red when dangled and pale when elevated. Prevalence around 15%
Main issue
Decreased blood flow means reduced nutrients resulting in reduced healing, increases pain which potentially leads to necrosis (death of tissue) and increase chance of amputation.
Neuroischaemic wounds
Presentation
This in a combination of both peripheral neuropathy and ischaemia (arterial
insufficiency) which leads to impaired tissue perfusion in a neuropathic diabetic foot.

Features
Typically occurs along the margins of the foot and toes.
Prevalence around 50%
Main issue
There is a degree of sensory loss due to the neuropathy and patient is prone to
necrosis due to the arterial insufficiency.
Venous wounds
Presentation
They have large, shallow, and irregular wound margins. Typically develop around the medial/lateral gator regions or ankle.
Features
Warm too touch, base is red and generally highly exudative (leaky wound). More often is painless/less painful than arterial ulcers, and oedema is usually present. Elevation of legs reduces symptoms and swelling as you are actively initiating venous return.
Main issue
Venous insufficiency = dysfunction of venous valves/deep vein thrombosis/heart failure which leads to a higher pressure within the peripheral veins and therefore increases pooling of venous blood resulting in blood not getting back to the heart.

Pressure wounds
Presentation
Initially starts off as a reddish blistered appearance. There are several stages (see photo or link of stages).
Features
There is an increased skin temperature to the affected region, mild discomfort and discoloured areas which do not turn white when there is pressure applied to the skin.
Main issue
Long standing pressure/shear/friction on the affected region in immobile/bed ridden patients reduces the blood supply to these tissues and therefore weakens the integrity of the skin and patient is susceptible to breaks due to the fragility.
Charcot neuropathic osteoarthropathy
Charcot neuropathic osteoarthropathy, typically referred as Charcot foot, affects the bones, joints and soft tissues of the foot and ankle region, where in the early stages cause the local inflammation that lead to different forms and patterns of bone destruction, subluxation and malformation of the foot bones in which the typical feature is a collapsed mid foot and “rocker bottom” foot (photo). A magnetic resonance imaging (MRI) is considered the best imaging technique in diagnoses if there is no clinical signs to discern between Charcot foot or an infection.

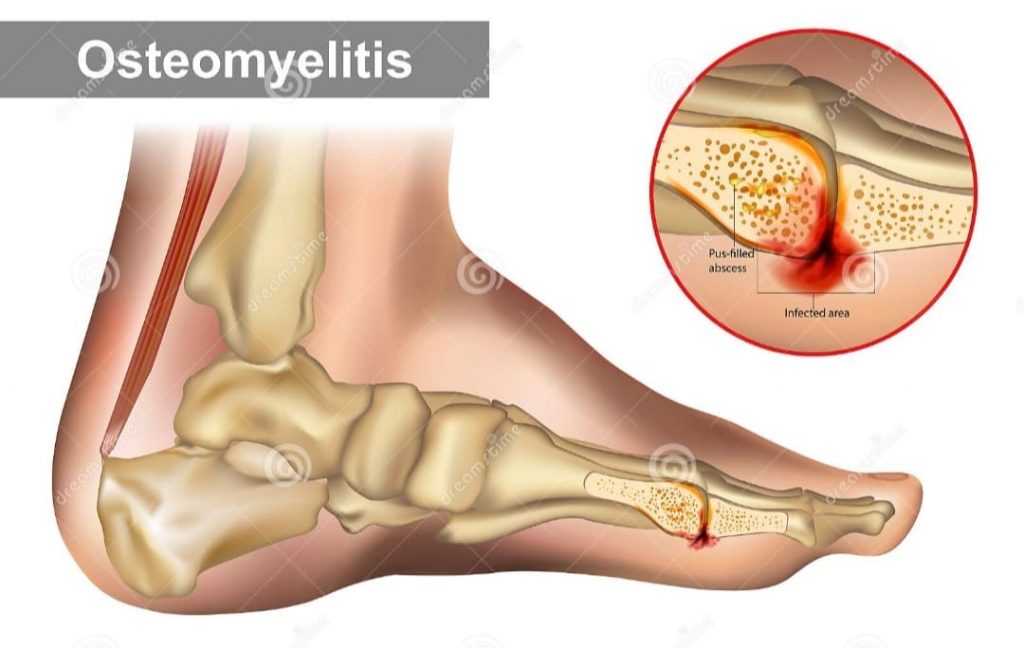
Osteomyelitis
Osteomyelitis is typically represented by “sausage toe” or visible bone. If unsure, a clinical test using a sterile blunt metal probe into the wound and checking for infection can be used to feel the bone underneath. Osteomyelitis can present in patients with moderate to severe diabetic foot infection. If osteomyelitis is not recognised and treated appropriately, the wound is not going to heal. Osteomyelitis can be hard to recognise initially as wounds that commonly overlie bony prominences, chronic, deep and large are susceptible to infection. Plain x-rays confirm diagnoses, but in the initial phase, if osteomyelitis is present it has low rate of picking infection up. If clinical suspicion is high and x-ray is negative, an MRI can
be used if not contraindicated.
Lower limb amputation
Lower extremity disease is a consequence of either peripheral neuropathy and/or peripheral arterial disease and is linked to a noticeably higher risk of amputation.
Individuals recently diagnosed or undiagnosed have an increase chance of amputation in contrast to non-diabetic population and even more risk if diagnosed longer than 10 years.
You can prevent complications occurring
The good news is, by looking after yourself and getting the appropriate health checks and knowledge from health professionals, it’s likely the complications can be prevented. Firstly, speak with your GP and check which health care providers you need at the current time and then utilise all health care settings available to you such as a podiatrist, diabetes educator, dietician, endocrinologist, and ophthalmologist.
Look at improving your lifestyle – a healthy diet advised by a dietician, keep active, and manage stress. Avoid alcohol, reduce weight if overweight and stop smoking if you are a smoker.
Home care tips :
-check feet daily for cuts and abrasions
-any cuts, clean with sterile saline and dress with a breathable dressing. Apply betadine solution if it appears inflamed or is throbbing. if its slow to heal, or inflammation increases, book asap with your podiatrist or gp.
-Wear well fitted footwear, with laces or velcro, firm heel counter and stiff shank, but flexible at the ball of the shoe, cushioned soles
– avoid putting your feet close to heaters
– apply heel balms to heel
– wash feet daily with warm water and gentle soap
It’s advised all diabetics get an annual diabetic foot health assessment, and attend their podiatrist on a regular basis to ensure skin and nail conditions are controlled, any infections or wounds are dealt with in a timely manner, and biomechanical inefficiencies are rectified. They will also advise on appropriate footwear and home care. This will help maintain your feet in good health and help prevent diabetic complications.
If you have diabetes, and have never seen a podiatrist, or have been recently diagnosed with diabetes, (or have a friend or relative that does), take advantage of the current special and get 40% off your initial assessments, only booked in with Will, for new patients only, until the end of March 2022. Mention this special .To book an appointment online at https://www.cheltenhampodiatry.com.au. or phone (03) 9583 3093 and see Will at Cheltenham podiatry for a thorough diabetes foot health check.
Book an appointment today
Latest News
Ankle Arthritis
Understanding Ankle Arthritis and Regenerative Treatment Options in Podiatry Ankle[…]