Telehealth Now available
bulkbilled through medicare and DVA where applicable *
bulkbilled through medicare and DVA where applicable *
What is a Lateral ankle sprain
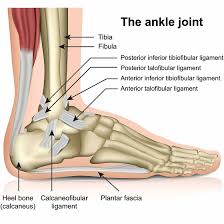
The foot and ankle is a complex piece of anatomy and design, with a multitude of ligaments, bones, and sinuses. A Lateral ankle sprain or ‘inversion ankle sprain’, is when you roll your ankle inwards, stretching and hurting the ligaments on the outside of your ankle joint. It is one of the most common injuries at this region, and one of the most common sports injuries.

The ankle joint consists of the tibia, fibula and talus articulating bones, and is stabilised mainly by three ligaments complexes : lateral complex (outside ankle), medial deltoid (inside of ankle ) and the Syndesmosis (high ankle area- between the fibular and tibia). Although there is a group of ligaments at the posterior (behind ) the ankle and just in front of the that can sometimes also be involved, in more severe injuries but is less common.
The severity of ankle sprains vary depending on the mechanism of injury ( high versus low energy), position of the foot and rotational force on the joint and stabilising ligamentous structures. Treatments and outcomes will also depend on the type of injury, damage , health and age.
The anterior talo fibular ligament ATFL is the first ligament to be damaged during a lateral ankle sprain, followed most often by the calcaneofibular ligament CFL. The posterior talo fibular ligament PTFL is the next one injured, but is typically only in severe ankle sprains and is often accompanied by fractures or dislocations or both. The calcanei cuboid and bifurcate ligaments, on the top of the foot and infront of the outside ankle, and the syndesmosis group high in the ankle, are less commonly injured.
Low grade injuries ( grade 1 and 2) result in stretching and or partial tears of the the ligaments, while a high grade (grade 3) ankle sprain often also includes the syndesmosis complex (tibia fibular ligaments structures) and may cause tendon disruption. Often, resulting in full ligament ruptures and fractures due to higher energy incidents.
You can also roll the other way and hurt the ligaments on the inside of your ankle, however, this is less common.
How do they occur?
Lateral ankle sprains most commonly occur due to excessive supination ( turning in) of the rear-foot about an externally (outwardly) rotated lower leg soon after initial contact of the rear-foot during gait or landing from a jump, often due to activity on uneven surfaces, poor footwear, and/or foot type.
This can result in strain to the lateral ankle ligaments. If the strain in any of the ligaments exceeds the tensile strength of the tissues, ligamentous damage occurs. Increased plantar flexion (forefoot and toes pointing down ) at initial contact appears to increase the likelihood of suffering a lateral ankle sprain.
There is high rate of recurrence reported and instability after sustaining a single primary ankle sprain, and 40 % report persistent symptoms, recurrent sprains, and chronic ankle instability, particularly if treatment is delayed, and/or the level of damage is not diagnosed accurately.
Who is most likely going to get them
The most common predisposition to suffering a lateral ankle sprain is the history of at least one previous ankle sprain. Perhaps the most frequently studied risk factor for lateral ankle-ligament sprains is a previous sprain of the lateral ankle. This is based on the fact that ligaments are an important joint stabilisers and damage can leave mechanical weaknesses at the ankle.
Research shows female athletes were at 25% increased risk of suffering a grade I ankle sprain compared with male athletes however, the relative risk between the sexes for the more serious grade II and III sprains, ankle fractures, and syndesmotic sprains was not significantly different.
Height and weight have been implicated as risk factors when an athlete is in an at-risk position for inversion ankle trauma, an increase in either height or weight proportionally increases the magnitude of inversion torque that must be resisted by the ligaments and muscles that span the ankle complex.
Limb dominance has been implicated as a risk factor for lower extremity trauma because most athletes place a greater demand on their dominant limb. Therefore, they produce increased frequency and magnitude of moments about the knee and ankle, particularly during high-demand activities that place the ankle and knee at risk.
Although literature states no one foot type has been identified as a risk factor, anecdotally or clinically I have seen patients with a high arched or supinated foot type more likely to have an inversion sprain. Evidence has suggested a link towards foot width showed that increased foot width is associated with an increased risk of suffering a sprain of the lateral ankle ligaments. This finding can be explained, at least in part, by the fact that during an inversion injury, an increased foot width is associated with an increased moment arm and corresponding inversion moment in comparison with a narrow foot.
To most professionals involved with the diagnosis and treatment of ankle injuries, increased joint laxity is considered a “sure bet” risk factor for an ankle injury because it indicates that a soft tissue restraint and its contribution to stability and neural intervention of the ankle complex may have been compromised. However, the literature presents conflicting findings.
How can you prevent them reoccurring
Early diagnosis and appropriate treatment is the best way to prevent reoccurrence. Cheltenham Podiatry is highly experienced in dealing with ankle sprains from mild to severe cases. Correct Diagnosis requires detailed assessment and appropriate diagnostics. We have onsite ultrasound for immediate assessment, but often patients will be referred for MRI, which is considered the gold standard for ankle injuries. Once correct diagnosis and level of injury is made, appropriate treatment will proceed. Where there are ligament ruptures healing can take up to 3 months and sometimes longer depending on all factors.
The natural progression of acute ankle sprains is a gradual improvement, as the initial symptoms of pain, swelling, and loss of function subside in the weeks after injury. The treatment plan will vary depending on grading of the injury. Complete ruptures require fibreglass casts for several weeks prior to rehabilitation, followed by bracing and regenerative treatments and graded rehabilitation program. Partial ruptures follow similar trajectory but no casting is required. It is crucial to continue and complete the full treatment plan (bracing and other therapies) combined with a rehabilitation for up 3 months or longer after their injury.

Rehabilitation programs should emphasise proprioceptive, neuromuscular control, and balance training to significantly reduce the risk of recurrent ankle sprains.
Some more severe graded injuries, will unfortunately require surgery where there are fractures involved , and /or instability and pain continuing following the treatment/rehabilitation program.
Ankle taping and bracing can be effective in preventing repetitive ankle sprains.

How can a podiatrist help with ankle sprains
Cheltenham Podiatry has an ankle sprain clinic, our podiatrists have up to date therapies and training to get you back to your activity and help prevent long term and reoccurring issues. We collaborate with surgeons to ensure we provide the best protocols to get you moving and healing as quick as possible. Treatment therapies often utilised in your plan will include:
To get to your goals contact Cheltenham Podiatry now, don’t delay your treatment.


Treating Baxter’s Nerve Entrapment: Conservative and Regenerative Treatments Understanding Baxter’s[…]
What Are Ingrown Toenails? Ingrown toenails, or onychocryptosis, occur when[…]